What would happen if we stopped telling nurses to be more resilient, and started changing the systems causing burnout in the first place?
That question has been at the heart of the Oregon Center for Nursing’s work since 2020, and it took center stage during our recent Friday Huddle: Extended Cut – Nurse Well-Being Webinar on November 14, 2025. In this 60-minute session, we shared key findings from the Well-Being Project, an initiative shaped by nurse-led pilot projects across Oregon. Days later we marked the official release of our new report, From Burnout to Belonging. The report, and the conversation it sparked, reflects a growing movement in Oregon: shifting from individual coping to organizational support and putting nurses at the center of designing what needs to change.
The origins of the Well-Being Project stemmed from a clear disconnect: what organizations were offering to support nurses wasn’t lining up with what nurses actually needed. Really needed. Our early surveys (and the ones that followed) made it plain: resilience training, wellness weeks, and mindfulness apps weren’t touching the root causes of stress and burnout. Nurses needed meaningful, systemic change. They wanted safer staffing, better communication, more aligned leadership, and work cultures that didn’t just talk about well-being, but built it into the infrastructure. That’s where this project began and where the conversation during our webinar continued.
From Self-Care to System Change
The RN Well-Being Webinar unpacked what we’ve learned from Oregon’s 18 nurse-led pilot projects: individual resilience is not a fix for organizational stress.
Panelists emphasized a shift toward system-level strategies, including:
Identifying removable stressors—aspects of the workplace that can be redesigned or eliminated
Supporting staff through manageable stressors, like compassion fatigue and moral misalignment
Listening intentionally to staff needs and co-creating practical changes
Throughout the session, speakers noted that many successful interventions began with a simple, powerful question: What is one stressor in your work environment that you wish could be removed today?
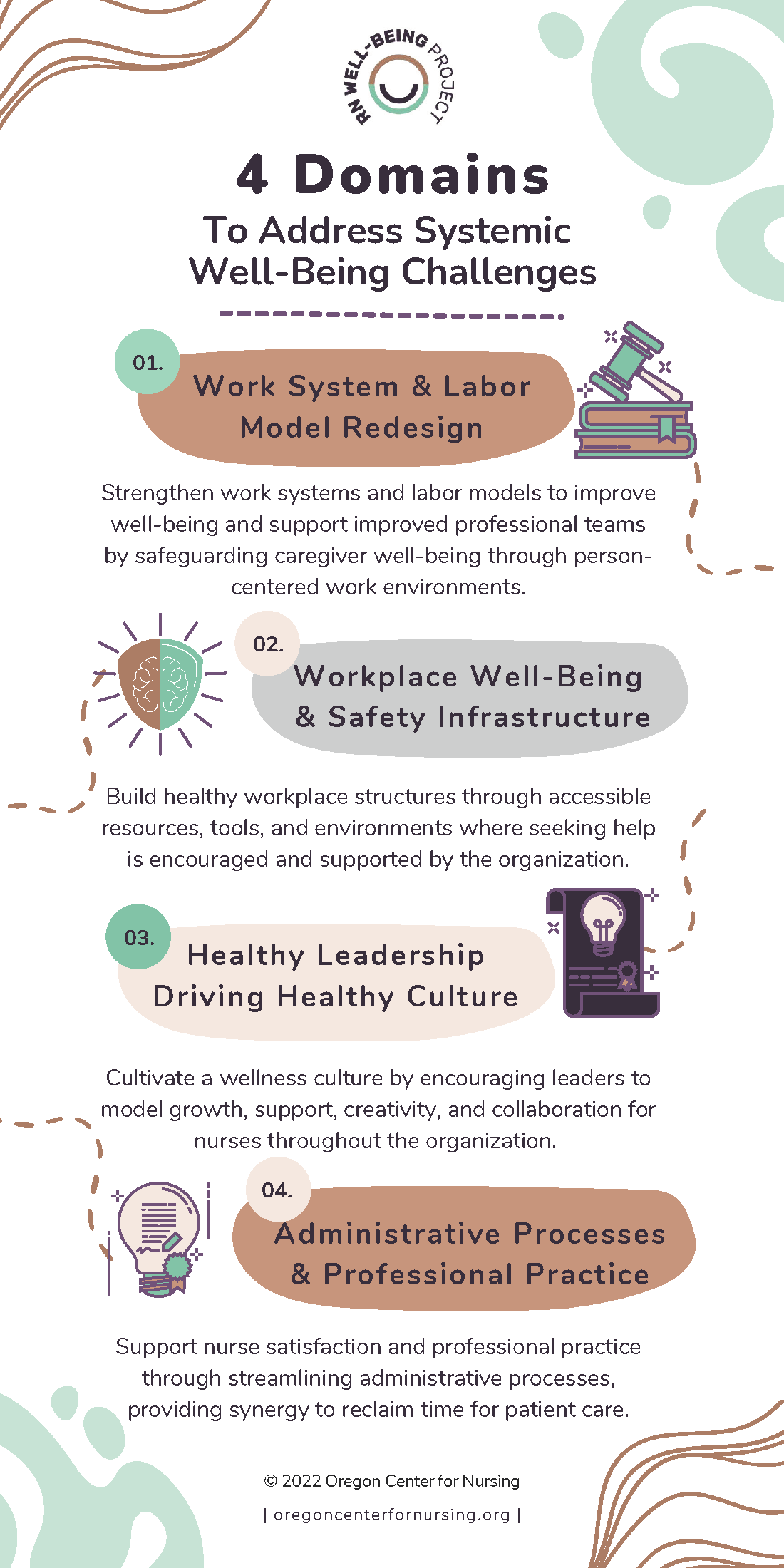
We also reviewed the four key domains (pictured left) used to guide and organize systems-level improvement across pilot sites.
Each domain is supported by printable guides and implementation tools, created for use by nurse leaders, managers, and executive decision-makers alike.
All of this (and more) is available now on our RN Well-Being Project microsite.
Tools for Managing Stressors
Of course, not all sources of stress can be removed. Some are deeply embedded in the work itself, such as witnessing trauma, navigating ethical gray areas, or carrying emotional weight long after a shift ends. These are what we call manageable stressors: the kinds of strain that require acknowledgment, support, and consistent system-level response.
During the webinar, we explored four of the stressors on our radar:
- Moral & Ethical Misalignment
- Vicarious Trauma
- Secondary Traumatic Stress
- Compassion Fatigue
Each of these shows up in different ways depending on the practice setting, but they share a common truth. These stressors signal that something in the system needs attention. This is why we created practical resources for each, and offer not just definitions, but strategies organizations can use to identify, talk about, and support staff working through these experiences.
All four resources are printable and ready to use, whether you’re starting a conversation in a team meeting, building leadership training, or rethinking how support shows up in policy. You can find them, along with other organizational tools, at wellbeing.oregoncenterfornursing.org.
While tools and frameworks are essential, lasting change starts with how leaders show up. One of the most grounded takeaways from the webinar came from our Executive Director, Jana Bitton, who said transformation isn’t about big programs. It’s about how we listen, respond, and lead.
“If you want to improve your well-being, go in with the right intention. Ask the staff—not often—but meaningfully. Be receptive to what they say. And pivot when you need to.”
Jana Bitton
One of the biggest lessons from this work – something we emphasized during the webinar – is the success of the Well-Being Project wasn’t about what the pilot sites did. The real story wasn’t found in any single initiative. What mattered was how they did it. As Jana beautifully put it, they began with the right intent, asked their staff what was needed, truly listened, and were willing to pivot along the way.
Each pilot site defined its own measures of success. Some reached those goals, some didn’t, but success wasn’t the only metric that mattered. When we surveyed participating nurses, we found when aggregated, they reported significantly lower stress indicators when compared to the broader state population survey in the same year. While the groups weren’t identical, and we can’t claim direct causation, it’s clear something worked. And given the wide variation across settings and strategies, the one constant was this: meaningful change happened when staff were included as co-creators.
If there’s one thing we hope leaders take away from the webinar and the report, it’s that the most powerful driver of change is a mindset, not a program or policy. Starting with intention, asking with purpose, listening closely, and adjusting along the way created the conditions for trust, participation, and progress even when the outcomes looked different across sites.
So what does all this mean in practice? It means, thankfully, you don’t need a consultant, a task force, or a big new budget to begin. You start with humility. With a willingness to ask your staff what’s really going on, to hear the hard parts, and to work together toward change. The most effective efforts we saw didn’t rely on elaborate frameworks. They relied on connection, trust, and a commitment to keep showing up, even when the answers weren’t easy.
OCN can support you in the journey to workplace well-being. The Well-Being Project wasn’t designed to prescribe one-size-fits-all solutions. It was built to offer flexible tools, shared language, and real-world examples to help you engage your teams and shape your own path forward.
What Leaders Can Do Now
Here are a few ways we can support you in continuing this work. Whether you’re leading a team, shaping policy, or influencing culture from within, these are entry points, resources and relationships, that can help you stay grounded in the approach we know makes a difference. Use what fits, adapt what doesn’t, and let us know how we can support you.
Start with the four domains and manageable stressors. These tools are available for download and use at your site.
We’re eager to speak with leadership teams, associations, boards, and community partners. Just ask!
- Champion the message
Share the report, use the talking points, and help normalize conversations about occupational well-being.
Let us know what you’ve tried, what’s needed, and what impact you’re seeing. What is one asset you wish we had available for you today? Let us know!
- Lean into each other
This is not a competition… it’s an evolution. Collaboration drives sustainable change.
Occupational well-being embedded into practice is rooted in listening, shared ownership, and the belief that the people closest to the work are essential to shaping its future. What we’ve learned through this project, and what we shared in the report and webinar, points to a simple truth: when we lead with trust and act with intention, meaningful change follows. However you choose to engage with this work, we hope you’ll see OCN as a partner in it.

Let’s Build a Culture Focused On Occupational Well-Being
With the release of From Burnout to Belonging, we’ve closed a chapter on our pilot projects. However, the work is just beginning.
In 2026, we’ll release:
Deeper analysis of practice settings and vulnerable populations from our 2025 survey
An infographic comparing 2022 and 2025 stress data
A leadership guidebook (manuscript nearing completion) to help health system leaders improve occupational well-being
Until then, everything we’ve built so far is available to you now, at no cost, and with no barrier.
Visit the microsite:
👉 wellbeing.oregoncenterfornursing.org
Explore the full report:
👉 Download From Burnout to Belonging
Watch the Recording:
👉 Friday Huddle Extended Cut: RN Well-Being
Questions? Want to collaborate?
Email us at outreach@oregoncenterfornursing.org

