A New View on Nurse Turnover: How the COVID-19 Pandemic Shocked the System
High nurse turnover rates were already a concern before COVID-19, but the pandemic introduced an unprecedented disruption to workforce stability. This publication explores how pandemic-related shocks altered nurses’ perceptions of job fit, community ties, and the value of staying. Understanding these shifts helps leaders better support retention and workforce cohesion.
Issues Facing the Post-Pandemic Nursing Workforce in Oregon – Stress and Emotional Health
Emotional fatigue and burnout continue to shape Oregon’s nursing workforce in the aftermath of COVID-19. This publication explores how stress, safety concerns, and organizational responses have impacted nurses’ well-being. With limited state-specific data, the report emphasizes the urgency of targeted support systems rooted in local realities.
Not Working Well: Clinical Placement for Nursing Students in an Era of Pandemic
Faced with the urgency of a global health crisis, nursing education programs and healthcare agencies in Oregon scrambled to adapt clinical placement strategies. This publication captures the resulting stress, innovation, and breakdowns that surfaced as traditional education pipelines were upended. Interviews across sectors reveal a critical moment of reckoning for how students are prepared for practice.
Issues Facing the Post-Pandemic Nursing Workforce in Oregon

COVID-19 intensified Oregon’s existing nursing workforce challenges, disrupting education pipelines and stressing care delivery systems. This report explores how these shifts affect nurse training, licensure trends, and frontline well-being. Nurse migration patterns and burnout risks reveal vulnerabilities that require immediate and strategic attention.
The Nurse Licensure Compact – a Primer
Debates around the Nurse Licensure Compact continue as states weigh the benefits of streamlined licensing against regulatory concerns. This primer explains the NLC’s mechanisms and outlines the arguments made in Oregon’s policy discussions. With multi-state licensure on the rise, understanding its implications remains vital for nursing leadership.
Nursing Maldistribution: The Intersection Between Practice Setting and Years of Nursing Experience
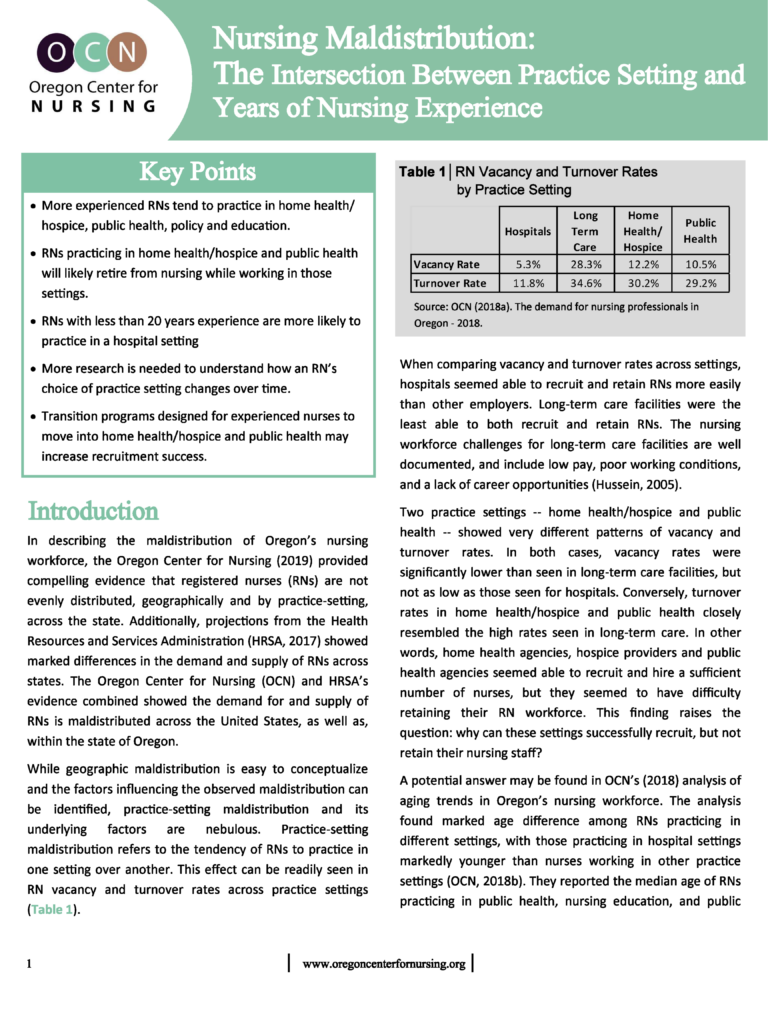
RNs across Oregon are not evenly distributed between care settings, especially when considering years of experience. Nurses with more experience tend to cluster in non-hospital environments, while newer nurses gravitate toward hospitals and long-term care. These patterns raise important implications for workforce planning, recruitment, and retention strategies statewide.
Primary Care Workforce Crisis Looming in Oregon: Nurse Practitioners Vital to Filling the Gap, But Not Enough to Go Around
Oregon faces an urgent primary care shortage, with only a fraction of nurse practitioners delivering direct primary care services. Despite favorable practice laws, the state struggles to align NP capacity with community needs. Policymakers must rethink workforce distribution to avoid deepening care disparities statewide.
Trends in Oregon Nursing Education 2012–18

Nursing education in Oregon is evolving, but not fast enough to meet projected workforce needs. While BSN programs are growing, ADN and LPN pathways show stagnation or decline. This analysis highlights long-term trends shaping the state’s ability to “grow its own” nursing workforce.
Shortage or Maldistribution: Shifting the Conversation About Oregon’s Nursing Workforce
Misconceptions about a statewide nursing shortage often overshadow a more pressing issue: maldistribution. This analysis reveals how workforce imbalance affects rural regions and non-hospital settings. OCN’s research encourages targeted action by identifying critical disparities in nurse availability across Oregon.
Nursing Apprenticeships: Examples for Oregon Discussion
Nursing apprenticeships are gaining renewed attention as a strategy to address workforce shortages in healthcare. This discussion paper explores existing models and evaluates their relevance to Oregon’s nursing pipeline. It invites healthcare leaders and policymakers to reimagine how education and on-the-job training can work together.
